Shop News
-
07/02/2025Colds & Flu - treatment and prevention
-
23/01/2025Curcumin Benefits
-
02/05/2024Ginseng - Nature's anti-inflammatory
-
02/05/2024Allergies Tradicional Chinese Medicine
-
12/03/2024Food Combining and Chinese Medicine
-
23/08/2023Phytoestrogens
-
05/06/2023Ginseng Benefits
-
02/06/2023Aumento de precios de la marca Blue Poppy
-
20/07/2022Infertility and Chinese Medicine
-
10/05/2022Allergic Rhinitis
-
24/03/2022TCM Obesity and Its Causes
-
23/03/2022Cancer Prevention and Diet
-
26/01/2022Medicinal Mushrooms
-
18/12/2021Christmas Remedies
-
15/10/2021Artemisia annua
-
09/07/2021CANDIDIASIS
-
03/03/2021Chinese Herbal Medicine formula studied to improve cancer therapy
-
12/01/2021The benefits of Xiao Yao San
-
15/09/2020Coronavirus Protocol (summary)
-
01/06/2020TCM Principles for Weight Loss
-
12/02/2020Take Good Care of Your Qi
-
01/01/2020Cordyceps Sinensis Benefits
-
01/12/2019Prevention & Treatment of Colds & Flu
-
27/04/2019ANXIETY - causes and treatments
-
26/03/2019Prostatitis and Chinese Herbs
-
01/03/2019What is an Adaptogenic Herb?
-
05/02/2019New Jade Herbal Formulas
-
09/12/2018The Shen of the Heart
-
23/08/2018Hyperthyroidism and Hypothyroidism
-
05/07/2018FOCUS ON A REMEDY: WARM THE MENSES
-
04/04/2018Treating Insomnia With Chinese Herbal Medicine
-
25/03/2018Cordyceps Sinensis research
-
01/03/2018Chinese Herbal Medicine for Panic Attacks
-
17/01/2018Clinical application of the Clear Metal remedy for advanced stage of influenza
-
02/01/2018New Pediatric Formulas by "Blue Poppy"
-
07/11/2017BI SYNDROME
-
01/09/2017Chemotherapy and Anti-Oxidants
-
05/03/2017Lumbar Disc Herniation
-
31/01/2017Treatment Principles in Exterior Invasions
-
21/10/2016Healthy Aging and Oriental Medicine: Qi is the secret
-
23/09/2016Horny Goat's Weed Benefits
-
25/08/2016Ganoderma Benefits
-
23/07/2016FOCUS ON A REMEDY: PROSPEROUS EARTH
-
25/06/2016Ginkgo Biloba Benefits
-
23/03/2016Blood Stasis
-
23/02/2016FOCUS ON A REMEDY: PROSPEROUS EARTH
-
23/01/2016CHRONIC FATIGUE SYNDROME
-
28/12/2015TONICS
-
24/10/2015A CASE HISTORY OF CHRONIC BRONCHITIS
-
23/09/2015Ganoderma Lucidum reduces obesity in mice
-
01/07/2015The Five Elements and Diet in Chinese Medicine
-
23/05/2015Daoist Sexual Practices
-
21/02/2015DEPRESSION
-
22/01/2015GLAUCOMA
-
20/12/2014ENDOMETRIOSIS
-
28/11/2014POLYCYSTIC OVARY SYNDROME
-
21/08/2014Ear infections and antibiotics
-
24/06/2014FOCUS ON A REMEDY: CHEMO-SUPPORT
-
21/03/2014Stomach-Yin Deficiency and Jade Spring
-
21/02/2014JOY, AN EMOTIONAL CAUSE OF DISEASE?
-
17/01/2014SEXUAL LIFE IN CHINESE MEDICINE
-
19/12/2013ON STAGNATION OF LUNG- AND HEART-QI
-
14/11/2013THREE TREASURES REMEDIES FOR PAIN
-
23/10/2013HEADACHE CASE HISTORY
-
22/10/2013.
-
12/07/2013Giovanni Maciocia Clinical Tip: Arouse Power
-
28/05/2013Blue Poppy - New Formulas
-
19/04/2013Case history - Chronic constipation
-
14/03/2013Three Treasures Webinar
-
31/01/2013Recurrent Bronchitis: a case history
-
31/12/2012FOCUS ON A REMEDY: SOOTHE THE SHEN
-
18/06/2012Herbs for the treatment of Anorexia
-
09/05/2012Three Treasures & Women's Treasures now available
-
09/04/2012REMEDY OF THE MONTH: CLEAR YANG
-
02/07/2011New Pediatric Formulas
-
28/04/2011Lingzhi slows progress of Alzheimer’s
-
18/10/2010European Legislation for natural products
-
19/09/2010700-year-old Chinese medicine can treat depression...
-
24/04/2010PDF Catalog
-
01/09/2009Swine Flue
 Chemotherapy and Anti-Oxidants
Chemotherapy and Anti-Oxidants
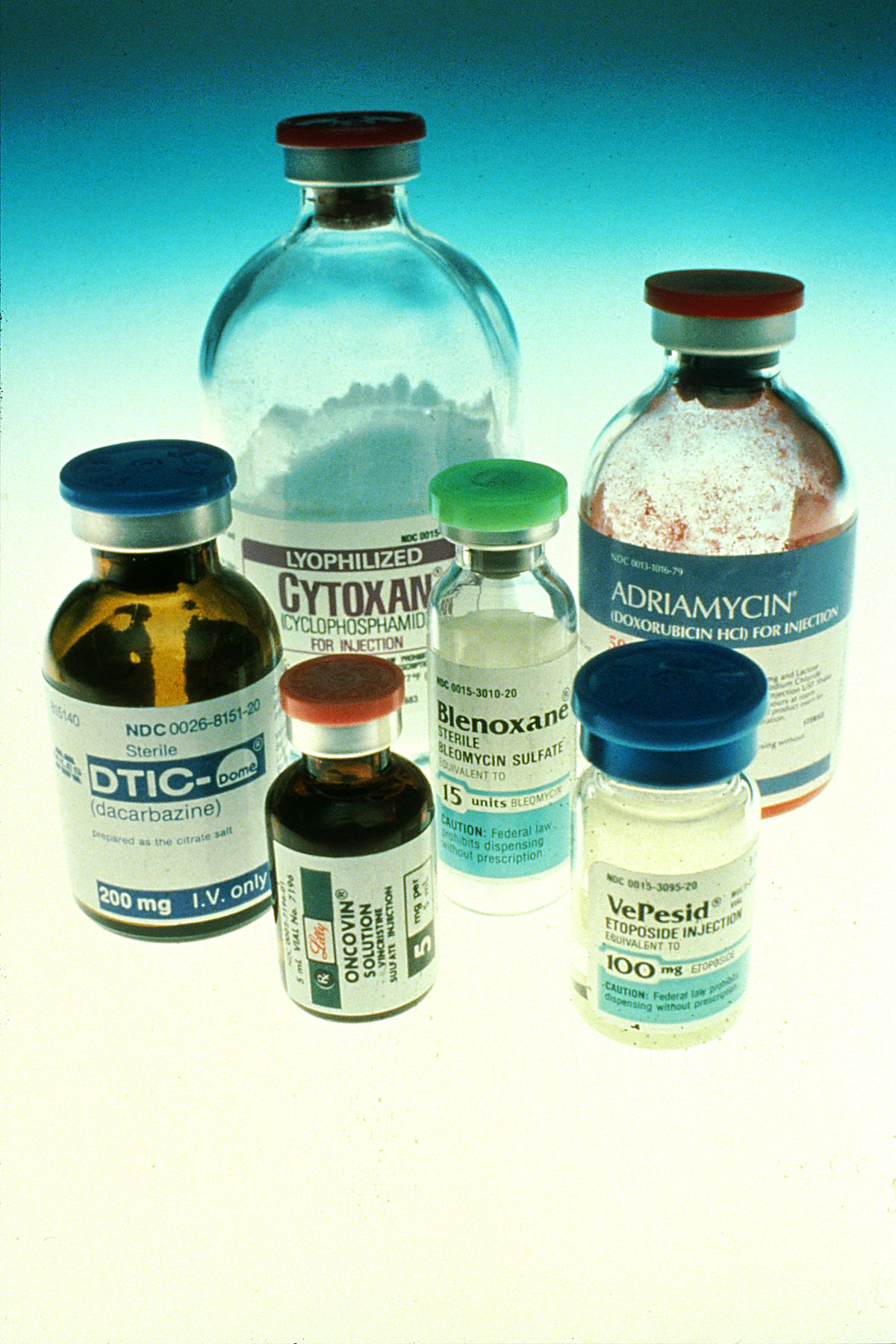
In the past few years it has become common practice by oncologists to advise patients who are undergoing chemotherapy not to take anti-oxidant supplements. The reasoning behind this advice is that chemotherapy destroys cancer cells by inducing free radicals and by promoting oxidation of the cancer cells. Antioxidants, on the contrary, do the exact opposite, i.e. they prevent free radicals (by binding to them) and the oxidation of cells. In theory, therefore, it would seem to follow logically that antioxidants may interfere with chemotherapy and reduce its effectiveness. As we shall see, in reality it is not as simple as that.
As oncologists also advise against the use of Chinese herbal remedies during chemotherapy, I shall approach this subject from two angles:
Whether it is true that anti-oxidants interfere with chemotherapy
Whether this applies to Chinese herbs
1. DO ANTI-OXIDANTS INTERFERE WITH CHEMOTHERAPY?
One particular article was influential in shaping the opinion that anti-oxidants interfere with chemotherapy. This was the article written by Dr Gabriella D'Andrea from the Memorial Sloan-Kettering Cancer Center, New York in Cancer Journal for Clinicians in 2005.
In this article, Dr D'Andrea states that, "mechanistic considerations suggest that antioxidants might reduce the effects of conventional cytotoxic therapies. Preclinical data are currently inconclusive and a limited number of clinical studies have not found any benefit. Clinicians should advise their patients against the use of antioxidant dietary supplements during chemotherapy or radiotherapy. Such caution should be seen as the standard approach for any unproven agent that may be harmful."
It is interesting that Dr D'Andrea agrees that "preclinical data are currently inconclusive" and yet she still comes to the conclusion that "clinicians shouldadvise their patients against the use of antioxidant dietary supplements during chemotherapy or radiotherapy." It is also interesting that she should attribute the opinion that antioxidants might reduce the effects of cytotoxic therapy to "mechanistic considerations": as we shall see, they are exactly that, i.e. "mechanistic".
Indeed, Dr D'Andrea takes a mechanistic view in saying "radiotherapy and many chemotherapy agents act by producing free radicals; some vitamins and supplements, including vitamins C and E, are antioxidants and bind to free radicals, preventing oxidative damage." She continues: "There are considerable in vitro and animal data showing that vitamin C and other antioxidants can protect cells against radiation and chemotherapy. It seems likely that they would therefore reduce treatment-related toxicities and there are promising, although not unequivocal, data that this indeed is the case. However, it also follows that antioxidants might protect cancer cells, thereby reducing the oncologic effectiveness of cytotoxic therapy. This is the reason why most oncologists discourage patients from using antioxidants during treatment."
However, Dr D'Andrea herself reports that "in vitro studies have reported that vitamins A, C, and E, as well as carotenoids, can enhance the effectiveness of chemotherapy and radiotherapy." Proponents of antioxidant therapy say exactly this, i.e. that the protective effects of antioxidants are selective for normal cells, such that they can reduce toxicities without compromising oncologic efficacy. They also say that antioxidants are directly cytotoxic and can actually increase the effectiveness of cytotoxic treatments.
Dr D'Andrea says that there are in vitro data suggesting a direct antitumor effect for vitamin C but she questions their validity. D'Incalci et al reviewed the literature on antioxidants and chemotherapy for the last 15 years and came to much more cautious conclusions than those reached by D'Andrea.
 D'Incalci et al say that "Studies have explored the effect of predominantly antioxidant vitamins and folate on efficacy or toxicity mediated by cisplatin and anthracyclins. Cisplatin toxicity in rodents was ameliorated by vitamin E. The design of clinical studies of dietary agents in combination with cytotoxic agents has been very heterogeneous and results have been inconclusive."ii They conclude cautiously that "whilst preclinical experiments hint at a potential benefit of certain dietary agents, the evidence emanating from clinical studies does not allow firm conclusions to be made. Future studies should explore physiological doses of dietary agent and include pharmacokinetic and pharmacodynamic measurements."iii
D'Incalci et al say that "Studies have explored the effect of predominantly antioxidant vitamins and folate on efficacy or toxicity mediated by cisplatin and anthracyclins. Cisplatin toxicity in rodents was ameliorated by vitamin E. The design of clinical studies of dietary agents in combination with cytotoxic agents has been very heterogeneous and results have been inconclusive."ii They conclude cautiously that "whilst preclinical experiments hint at a potential benefit of certain dietary agents, the evidence emanating from clinical studies does not allow firm conclusions to be made. Future studies should explore physiological doses of dietary agent and include pharmacokinetic and pharmacodynamic measurements."iii
Other researchers too contest D'Andrea's conclusions. They maintain that antioxidants given during chemo- and radio-therapy induce apoptosis, a process whereby cancer cells die off in a natural manner. Cancer cells that die off due to apoptosis are literally digested and removed by phagocytes, thus preventing the inflammatory response induced by chemotherapy. By contrast, oxidation induced by chemotherapy kills cancer cells in a manner that results in masses of dead cells (with broken membranes) that produce inflammation and toxic response.
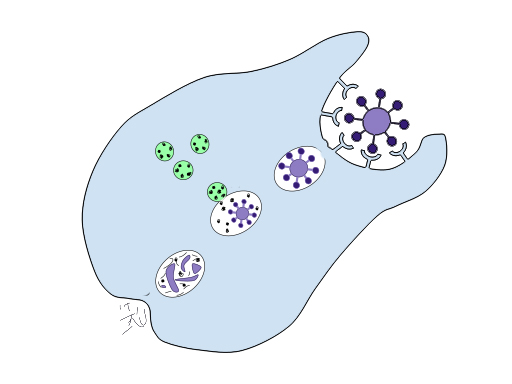
All cells have a finite life span and cell death occurs mainly as a result of passive necrotic processes or due to an active process of programmed cell death, "apoptosis". Apoptosis is the most common mechanism by which the body eliminates damaged or unneeded cells without local inflammation from leakage of cell contents.
Cells that are undergoing apoptosis exhibit a characteristic pattern of morphologic changes, including cell shrinkage, condensation, fragmentation of the nucleus and bubbling of the plasma membrane, known as "blebbing", chromatin condensation and nucleosomal fragmentation. The resulting membrane-bound apoptotic bodies are consumed by neighboring cells or by macrophages. In contrast, the necrotic mode of cell death represents a passive consequence of mechanical damage or exposure of the cells to toxins (such as chemotherapy).
However, some antineoplastic drugs kill tumor cells by inducing apoptosis. As described above, this highly controlled mechanism of cell death is thought to be physiologically advantageous because apoptotic cells are removed by phagocytosis before they lose their permeability barrier, thus preventing induction of an inflammatory response to the dying cells. In contrast, necrotic cells lyse and release their contents into the extracellular space, thus inducing inflammation.
Shacter et al examined the effects of oxidative stress on chemotherapy-induced cell killing. They found that H2O2 (hydrogen peroxide) inhibits the ability of four different chemotherapy drugs (VP-16, doxorubicin, cisplatin, and AraC) to induce apoptosis in human Burkitt lymphoma cells. H2O2 shifts the form of cell death from apoptosis to pyknosis/necrosis, which occurs after a significant delay compared with chemotherapy-induced apoptosis. It can also lower the degree of cell killing by these drugs. These effects of H2O2 can be prevented by the antioxidant agents Desferal, Tempol, and dimethylsulfoxide.
Phagocytosis by monocyte-derived macrophages of VP-16-treated lymphoma cells is also inhibited by H2O2. Cells killed with H2O2 (with or without VP-16) do ultimately undergo phagocytosis, but this occurs only after they have lost their permeability barrier. Thus, membrane-intact apoptotic cells are recognized and phagocytosed by monocyte-derived macrophages, but membrane-intact pyknotic/necrotic cells are not. The results suggest that chemotherapy-induced apoptosis and phagocytosis of cancer cells may be enhanced by including certain antioxidant agents in the treatment protocol.iv
In other words, there are situations when the oxidative stress induced by chemotherapy itself may actually hinder the effects of chemotherapy and the addition of antioxidants may actually help chemotherapy to work in a more natural, non-inflammatory way (i.e. through apoptosis rather than necrosis).
Dr Kenneth Conklin confirms this in his article "Chemotherapy-Associated Oxidative Stress: Impact on Chemotherapeutic Effectiveness".v In this article, Dr Conklin says that "Antineoplastic agents induce oxidative stress in biological systems. During cancer chemotherapy, oxidative stress-induced lipid peroxidation generates numerous electrophilic aldehydes that can attack many cellular targets. These products of oxidative stress can slow cell cycle progression of cancer cells and cause cell cycle checkpoint arrest, effects that may interfere with the ability of anti-cancer drugs to kill cancer cells. The aldehydes may also inhibit drug-induced apoptosis by inactivating death receptors and inhibiting caspase activity [the latter would slow down cell disassembly]. These effects would also diminish the efficacy of the treatment. The use of antioxidants during chemotherapy may enhance therapy by reducing the generation of oxidative stress-induced aldehydes.
Dr Conklin also conducted a study on patients who were receiving chemotherapy (anthracyclines) for breast cancer and lymphoma. Co-enzyme Q10 was administered in conjunction with chemotherapy. Results showed that the administration of Q10 resulted in fewer cardiomyopathy (a side-effect of anthracyclines). Dr Conklin says in the summary of the study: "There is concern within the oncology community that consumption of antioxidants during chemotherapy will reduce the effectiveness of the treatment. Cytotoxic antineoplastic agents generate reactive oxygen species (ROS) in biological systems and many oncologists contend that this accounts for, or contributes to, the anti-cancer activity of the drugs. However, all of the drugs have [their own] established mechanisms of action that do not depend [always] upon their production of ROS. ROS can reduce the efficacy of chemotherapy because they interfere with cell cycle progression and apoptotic mechanisms. Thus, antioxidants should not interfere with the mechanism of action of antineoplastic agents, and may enhance their effects by preventing the impact of ROS on the cell cycle and apoptosis. The results of the present study support the contention that antioxidants do not interfere with the anti-cancer effects of antineoplastic agents. Additionally, the administration of co-enzyme Q10 during the patients' anthracycline-based chemotherapy appears to have prevented any cardiac damage."
Block et al also reviewed the literature on antioxidants and chemotherapy and came to the same conclusion. Dr Block, of the Block Center for Integrative Cancer Treatment, says: "This review demonstrates that there is no scientific support for the blanket objection to using antioxidants during chemotherapy. In addition, it also appears that these supplements may help mitigate the side effects of chemotherapy."
The study considered 845 articles and 19 trials met the inclusion criteria. Antioxidants evaluated were: glutathione (7), melatonin (4), vitamin A (2), an antioxidant mixture (2), vitamin C (1), N-acetylcysteine (1), vitamin E (1) and ellagic acid (1). Subjects of most studies had advanced or relapsed disease.
The conclusion was that none of the trials reported evidence of significant decreases in efficacy from antioxidant supplementation during chemotherapy. Many of the studies indicated that antioxidant supplementation resulted in either increased survival times, increased tumor responses, or both, as well as fewer toxicities than controls. 15 of 17 trials that assessed chemotherapy toxicities, including diarrhea, weight loss, nerve damage and low blood counts, concluded that the antioxidant group suffered similar or lower rates of these side effects than the control group.
Co-author Dr. Robert Newman, Professor of Cancer Medicine at M. D. Anderson Cancer Center said, "This study, along with the evolving understanding of antioxidant-chemotherapy interactions, suggests that the previously held beliefs about interference do not pertain to clinical treatment."ix The authors noted that reducing side effects may help patients avoid having to cut back on their chemotherapy dosing, interrupt scheduled treatments, or abandon treatment altogether. This in turn, is likely to favorably impact treatment outcomes.
2. CHINESE HERBS AND CHEMOTHERAPY
How does this affect the use of Chinese herbs during chemotherapy? Much of the above discussion on antioxidants and chemotherapy actually does not apply to Chinese herbs as they contain few antioxidants and in doses that would be akin to those found in foods. Beta-carotene, for example, is a powerful antioxidant. Beta-carotene is found in carrots, sweet potatoes, kale, spinach, winter squash, cilantro (coriander) and thyme.
Only Hypericum (St John's Wort) may present some interaction with chemotherapy. In fact, this herb lowers the availability of some drugs as it activates the drug-metabolizing enzyme cytochrome P450 CYP3A4. Hypericum is used in Chinese medicine but not widely and it is not included in Chemo-Support. Very few Chinese herbs contain Vit C and, if they do, it would be in minimal doses.
The only ingredient of Chemo-Support that has a mild antioxidant effect is Dang Gui Radix Angelicae sinensis: considering this is only one out of 16 ingredients, the overall antioxidant effect of Chemo-Support is negligible. In conclusion, eating 2 pound of carrots, drinking a glass of orange juice and a cup of green tea would deliver far more antioxidants than 6 tablets of Chemo-Support. There is therefore absolutely no justification for recommending not to take Chemo-Support while on chemotherapy.
3. CHEMO-SUPPORT: PROTOCOL AND DOSAGE
Chemo-Support works better if it is started some time before the beginning of chemotherapy and continued for about 4 weeks after the end. It is important to note that "during the treatment" means during the course of treatment, i.e. also in the days of break from the treatment. The dosage is as follows:
Two weeks before the start of treatment: 3 tablets a day
Four days before the start of treatment: 2 tablets twice a day
During the treatment: 3 tablets three times a day
After the end of treatment for 4 weeks: 2 tablets twice a day
It is best to take the tablets away from meals, i.e. about 1 hour before or after a meal, swallowed with hot water. The tablets should also be taken separately from other medication, at least 1 hour away. If the patient feels very nauseous and finds it difficult to swallow the tablets, these could be crushed and powdered, immersed in a small amount of hot water with three slices of fresh ginger and the water sipped slowly.
The dosage during treatment indicated above should be adjusted according to the severity of the side-effects and the above dosage could be reduced or increased.
If the patient is receiving both chemo- and radio-therapy and is taking both Chemo-Support and Radio-Support, the dosage of each should be reduced. Adjustments can be made according to the patient's side-effects and timing of therapies in this situation by using a higher ratio of Chemo-Support during the days surrounding chemotherapy or when its side-effects are heightened. Similarly, the dosage of Radio-Support can be increased if the side-effects experienced from radiotherapy are more severe, or during the days surrounding the administration of radiotherapy.
Chemo-Support should be discontinued approximately four weeks after the end of the treatment when the condition should be reassessed and a different formula given. By contrast, Radio-Support should be continued for at least 6 weeks after the end of radiotherapy.
In the past 2-1/2 years, I have been diagnosed with rectal cancer and liver cancer metastases. I am a 52-year old man. Throughout my treatment, which has been, to say the least, extremely challenging, I have received acupuncture treatments regularly to relieve the side effects of my chemotherapy and to help me heal from my surgeries.
However, although I have weathered my treatments pretty well, I was continuing to get more and more fatigued with foggy thinking and was beginning to have severe digestive issues.
"My acupuncturist prescribed Chemo-Support to help me with these side effects. When I began to take it (in the weeks between my semi-monthly chemotherapy) I noticed almost immediately that I was able to think clearer and to feel stronger. In fact, with each subsequent chemo treatment I seem to be more resilient, having less severe reactions to those treatments with more restful sleep, no more digestive issues. My quality of life has improved tremendously overall, between the acupuncture and now, because of the Chemo-Support."
C.S.
"I have treated over twenty patients with Chemo-Support for an average of four to six months. I have observed and my patients have reported to find Chemo-Support beneficial for improving energy and in decreasing the side effects of nausea and vomiting."
Lucy Postolova, L.Ac.
Los Angeles, CA
"At [our] clinic we use both Chemo-Support and Radio-Support for many of our patients. I have definitely seen less fatigue in the women I have treated with Chemo-Support. They report that their energy and stamina are improved and there is less occurrence of anemia associated with chemotherapy. One of my patients was referred to me after she had undergone two rounds of chemotherapy. She was exhausted, very depressed, and felt very dry and depleted. She was on Chemo Support for the last round of therapy and she felt much less exhausted, her energy increased and she had fewer sensations of heat and night sweating."
Robin Germain, L.Ac.
San Francisco, CA
"I have been treating several women with breast cancer who have been undergoing chemotherapy. The patient who is taking Chemo-Support has had considerable improvement with her digestive function. Prior to taking Chemo-Support, she was suffering from burning, painful diarrhea which is no longer a problem. She is very pleased with her herbal treatment."
Dianne Gobrogge, L.Ac.
Wilmington, NC
"We find Chemo-Support to be beneficial in the initial treatment of Stage I and Stage II breast cancer, and especially in combination with other formulas (such as Brocade Sinews with Chemo Support for use with Taxol and Glorious Sea and Chemo-Support when using Navelbine). Along with acupuncture, Chemo-Support is helpful in supporting the Qi and helping the patient tolerate chemotherapy."
Beverly Burns, L.Ac.
San Francisco, CA
By: Giovanni Maciocia