Shop News
-
25/11/2025Ganoderma Benefits
-
07/02/2025Colds & Flu - treatment and prevention
-
24/01/2025Ginseng - Nature's anti-inflammatory
-
23/01/2025Curcumin Benefits
-
02/05/2024Allergies Tradicional Chinese Medicine
-
12/03/2024Food Combining and Chinese Medicine
-
23/08/2023Phytoestrogens
-
05/06/2023Ginseng Benefits
-
02/06/2023Aumento de precios de la marca Blue Poppy
-
20/07/2022Infertility and Chinese Medicine
-
10/05/2022Allergic Rhinitis
-
24/03/2022TCM Obesity and Its Causes
-
23/03/2022Cancer Prevention and Diet
-
26/01/2022Medicinal Mushrooms
-
18/12/2021Christmas Remedies
-
09/07/2021CANDIDIASIS
-
03/03/2021Chinese Herbal Medicine formula studied to improve cancer therapy
-
12/01/2021The benefits of Xiao Yao San
-
15/09/2020Coronavirus Protocol (summary)
-
01/06/2020TCM Principles for Weight Loss
-
12/02/2020Take Good Care of Your Qi
-
01/01/2020Cordyceps Sinensis Benefits
-
01/12/2019Prevention & Treatment of Colds & Flu
-
27/04/2019ANXIETY - causes and treatments
-
26/03/2019Prostatitis and Chinese Herbs
-
01/03/2019What is an Adaptogenic Herb?
-
05/02/2019New Jade Herbal Formulas
-
09/12/2018The Shen of the Heart
-
23/08/2018Hyperthyroidism and Hypothyroidism
-
05/07/2018FOCUS ON A REMEDY: WARM THE MENSES
-
04/04/2018Treating Insomnia With Chinese Herbal Medicine
-
25/03/2018Cordyceps Sinensis research
-
01/03/2018Chinese Herbal Medicine for Panic Attacks
-
17/01/2018Clinical application of the Clear Metal remedy for advanced stage of influenza
-
02/01/2018New Pediatric Formulas by "Blue Poppy"
-
07/11/2017BI SYNDROME
-
01/09/2017Chemotherapy and Anti-Oxidants
-
05/03/2017Lumbar Disc Herniation
-
31/01/2017Treatment Principles in Exterior Invasions
-
21/10/2016Healthy Aging and Oriental Medicine: Qi is the secret
-
23/09/2016Horny Goat's Weed Benefits
-
23/07/2016FOCUS ON A REMEDY: PROSPEROUS EARTH
-
25/06/2016Ginkgo Biloba Benefits
-
23/03/2016Blood Stasis
-
23/02/2016FOCUS ON A REMEDY: PROSPEROUS EARTH
-
23/01/2016CHRONIC FATIGUE SYNDROME
-
28/12/2015TONICS
-
24/10/2015A CASE HISTORY OF CHRONIC BRONCHITIS
-
23/09/2015Ganoderma Lucidum reduces obesity in mice
-
01/07/2015The Five Elements and Diet in Chinese Medicine
-
23/05/2015Daoist Sexual Practices
-
21/02/2015DEPRESSION
-
22/01/2015GLAUCOMA
-
20/12/2014ENDOMETRIOSIS
-
28/11/2014POLYCYSTIC OVARY SYNDROME
-
21/08/2014Ear infections and antibiotics
-
24/06/2014FOCUS ON A REMEDY: CHEMO-SUPPORT
-
21/03/2014Stomach-Yin Deficiency and Jade Spring
-
21/02/2014JOY, AN EMOTIONAL CAUSE OF DISEASE?
-
17/01/2014SEXUAL LIFE IN CHINESE MEDICINE
-
19/12/2013ON STAGNATION OF LUNG- AND HEART-QI
-
14/11/2013THREE TREASURES REMEDIES FOR PAIN
-
23/10/2013HEADACHE CASE HISTORY
-
22/10/2013.
-
12/07/2013Giovanni Maciocia Clinical Tip: Arouse Power
-
28/05/2013Blue Poppy - New Formulas
-
19/04/2013Case history - Chronic constipation
-
14/03/2013Three Treasures Webinar
-
31/01/2013Recurrent Bronchitis: a case history
-
31/12/2012FOCUS ON A REMEDY: SOOTHE THE SHEN
-
18/06/2012Herbs for the treatment of Anorexia
-
09/05/2012Three Treasures & Women's Treasures now available
-
09/04/2012REMEDY OF THE MONTH: CLEAR YANG
-
02/07/2011New Pediatric Formulas
-
28/04/2011Lingzhi slows progress of Alzheimer’s
-
18/10/2010European Legislation for natural products
-
19/09/2010700-year-old Chinese medicine can treat depression...
-
24/04/2010PDF Catalog
-
01/09/2009Swine Flue
Prostatitis and Chinese Herbs
The main symptoms are:
Painful urination
And scanty dark urine;
Pain in the genital area;
Low back pain;
Sexual dysfunction;
Fatigue and depression;
The prostate is a reproductive gland located below the bladder and in front of the rectum. Surrounds the urethra, the tube that carries urine from the bladder.
The prostate is the main producer of male semen.
To diagnose prostatitis, a physician must examine the patient's urine and the prostate through the rectal examination. He may also need to Recollect a sample of prostate fluid for analysis.
Prostatitis can be bacterial, nonbacterial acute and chronic.
 The most common is non-bacterial. Symptoms may include frequent urination and pain in the lumbar region.
The most common is non-bacterial. Symptoms may include frequent urination and pain in the lumbar region.
The causes of this type of prostatitis may be stress and irregular sexual activity.
The treatment for this type of prostatitis may include anti-inflammatory drugs, muscle relaxants, diet changes, fluid intake, and ejaculating frequently.
Acute bacterial prostatitis usually results from a bacterium or virus, or sexually transmitted diseases. Symptoms may include fever, pain in lower back, frequent urination and pain during urination, small amounts of urine and iregular urination.
These types of prostatitis are usually treated with antibiotics, fluids, and treatment for constipation.
Chronic prostatitis may be bacterial or the result of inflammation of the prostate.
Symptoms include frequent bladder infections, frequent urination and persistent pain in the abdomen or back.
This type of prostatitis is usually treated with antibiotics, dietary changes and supplements.
Treatments Chinese Herbal Medicine: 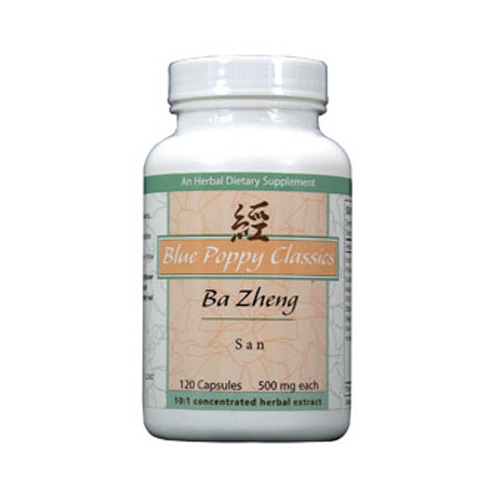
A treatment with excellent results is the herbal formula Ba Zheng San .
The actions of this formula in TCM are: Clear Dampness, heat and clear toxins. Purging pathogenic fire and relieve the stranguria.
This formula is used primarily to treat symptoms caused by heat in the Lower Jiao, aggravated by strangury hematuria, dysuria, abdominal distension, layer of yellow or red tongue and slippery pulse.
Among the modern treatments are included: urinary tract infections, cystitis, pyelitis, urolithiasis, prostatitis, kidney stones, etc.
The ingredients are:
Da Huang, Gan Cao, Che Qian Zi, Zhu Ling, Qu Mai, Zhi Zi, Hua Shi
Pharmacology:
Antibacterial effect: this formula has been shown to have a bacteriostatic effect on gonococcus with minimum inhibitory concentration less than 20 mg / ml. At 100 mg / ml, the formula can kill the gonococcus in 10 minutes, but the formula does not directly inhibits elcolibacillus urinary pathogens, which makes is to inhibit the adhesion of pathogens of urinary tract colibacillus and epithelial cells and therefore has the effect treatment of urinary tract infections caused by urinary pathogens colibacillus.
When administered to mice with cystopyelonephritis (bladder inflammation) Ba Zheng San increases urination and eliminates pathogenic bacteria in the urinary tract in the kidney. This formula can also increase the survival rate of rats infected with Proteus colibacilus mice.
Ba Zheng San has a bacteriostatic effect on the following bacteria: Staphylococcus aureus, Staphylococcus epidermidis, Pseudomonas aeruginosa, Bacillus coli, Bacillus Proteus bacillus Flexner, Shiga Bacillus, Serratia marcescens, etc.
Prevention of urinary calculi: in vitro experiments showed that Ba Zheng San can inhibit or prevent crystallization and prevent the calculation of calcium oxalate is formed.
Clinical trials:
106 cases of various urinary tract infections were treated with Ba Zheng San in clinical studies. The results showed that the formula is effective in treating various types of urinary tract infections and prostatitis.
What is an Adaptogenic Herb?
Adaptogenic herbs have unique properties that help soothe the soul while also providing the strength and vitality required  for sustained physical or mental activity when needed. Adaptogenic herbs work to improve the body’s ability to adapt to stress, giving you energy, yet also allowing for clarity and calmness.
for sustained physical or mental activity when needed. Adaptogenic herbs work to improve the body’s ability to adapt to stress, giving you energy, yet also allowing for clarity and calmness.
For centuries, adaptogenic herbs have been used to prevent and treat a wide variety of conditions. Known to help regulate the adrenal system, they can reduce levels of cortisol, the hormone that the adrenals produce during times of stress. prolonged high levels of cortisol due to chronic stress can be detrimental, leading to a wide range of health concerns, including poor sleep, autoimmune diseases, depression, anxiety, common colds and flu, hormone imbalance, cancer, thyroid conditions and digestive problems.
If you google "adaptogens, pubmed studies," thousands of entries will show up. The herbs that fall into this category have been used for thousands of years, but it was only in the late 1940s that a Russian scientist adopted the word "adaptogenic" to categorize them. A study published in 1999 defined an adaptogenic compound as a non-specific remedy "that increases resistance to a broad spectrum of harmful factors (stressors) of different physical, chemical and biological natures."
Some of the most common adaptogenic herbs are:
Cordyceps (cordyceps sinensis)
Chinese Ginseng / Korean (panax ginseng)
Astragalus (Astragalus membranaceus)
Siberian Ginseng (eleutherococcus senticosus)
Other hierbas adaptogenic herbs present in various formulas:
Dang shen (codonopsis pilosula, c. tangshen)
Licorice (glycyrrhiza glabra, g. uralensis)
Rhodiola (Rhodiola rosea)
Schisandra (schisandra chinensis)
Ashwagandha (Withania somnifera)
New Jade Herbal Formulas
JADE HERBAL products are safe and easy to use. The formulas are based on well-known traditional herbal combinations and have been specially adapted to our Western way of life.
Presented in 500mg tablets, with a concentration of 5: 1, which means that each tablet is equivalent to 2500mg.
The dosage is variable depending on the condition to be treated, as a minimum dose we advise 2 to 3 tablets, 2 times a day.
The Shen of the Heart

The Shen of the Heart plays a prominent role in memory partly by itself and partly because it coordinates the Yi of the Spleen and the Zhi of the Kidneys which also play a role in memory.
The Shen of the Heart plays a role in memory in the sense of memorizing but especially also in intrinsic memory (see below).
Information that we have to consciously work to remember is known as explicit memory, while information that we remember unconsciously is known as implicit memory. Implicit memory is not always unconscious as it includes what we call "muscle memory" which in psychology is called "procedural memory" (see below).
Explicit Memory
When we are trying to intentionally remember something (like the names of acupuncture points or a list of dates for a history class), this information is stored in our explicit memory. We use these memories every day, from remembering information for a test to recalling the date and time of a doctor's appointment. This type of memory is also known as declarative memory, since we can consciously recall and explain the information.
Some tasks that require the use of explicit memory include remembering what we learned in a class, recalling a phone number, writing a research paper, and remembering what time we are meeting a friend, etc.
There are two major types of explicit memory:
1. Episodic memory: These are our long-term memories of specific events, such as what we did the day before or our high school graduation.
2. Semantic memory: These are memories of facts, concepts, names, and other general knowledge information.
Implicit Memory
Things that we do not purposely try to remember are stored in implicit memory. This kind of memory is both unconscious and unintentional. Implicit memory is also sometimes referred to as non-declarative memory, since we are not able to consciously bring it into awareness.
Procedural memories, such as how to perform a specific task like swinging a baseball bat or sewing, are one type of implicit memory since we do not have to consciously recall how to perform these tasks. While implicit memories are not consciously recalled, they still have an influence on how we behave as well as our knowledge of different tasks.
Some examples of implicit memory include singing a familiar song, typing on our computer keyboard, daily habits, driving a car, riding a bicycle, sewing.
Riding a bicycle is another great example. Even after going years without riding one, most people are able to hop on a bike and ride it effortlessly.
The Shen of the Heart plays a role in both extrinsic and intrinsic memory but it is especially the one that is responsible for intrinsic memory, which the Yi of the Spleen and the Zhi of the Kidneys are not.
Heart-Blood deficiency and Heart-Yin deficiency are a common cause of poor memory.
.jpg?1543916733403)
HEART-BLOOD DEFICIENCY
Palpitations, dizziness, insomnia, dream-disturbed sleep, poor memory, anxiety, propensity to be startled, dull-pale complexion, pale lips.
Tongue: Pale, Thin, slightly dry.
Pulse: Choppy or Fine.
Key symptoms: palpitations, insomnia, poor memory, Pale tongue.
Acupuncture
Points: HE-7 Shenmen, Ren-14 Juque, Ren-15 Jiuwei, Ren-4 Guanyuan, BL-17 Geshu (with moxa), BL-20 Pishu.
Method: all with reinforcing method. Moxa can be used.
HEART-YIN DEFICIENCY
Palpitations, insomnia, dream-disturbed sleep, propensity to be startled, poor memory, anxiety, mental restlessness, dry mouth and throat, night sweating.
Tongue: no coating, deep midline crack reaching the tip.
Pulse: Floating-Empty.
Key symptoms: palpitations, mental restlessness, night-sweating, tongue without coating.
Acupuncture
Points: HE-7 Shenmen, Ren-14 Juque, Ren-15 Jiuwei, Ren-4 Guanyuan, HE-6 Yinxi, SP-6 Sanyinjiao.
Method: all with reinforcing method, no moxa.
THE YI OF THE SPLEEN
The Chinese character for the mental aspect of the Spleen is Yi which can mean "idea" or "intention".
The Yi resides in the Spleen and is responsible for applied thinking, studying, memorizing, focusing, concentrating and generating ideas.
The Post-Natal Qi and Blood are the physiological basis for the Yi. Thus if the Spleen is strong, thinking will be clear, memory good and the capacity for concentrating, studying and generating ideas will also be good.
If the Spleen is weak, the Yi will be dull, thinking will be slow, memory poor and the capacity for studying, concentrating and focusing will all be weak.
The Spleen is responsible for memory in the sense of studying, concentrating, focusing and memorizing data in the course of one's study or work.
Note that the Chinese character for "Yi" is based on the "heart" radical. This indicates two things. Firstly, it indicates that the memory of the Spleen depends also on the Heart. Secondly, it refers to the Shen's coordinating and integrating function in respect of the Hun, Po, Yi and Zhi.
SPLEEN-BLOOD DEFICIENCY
Poor appetite, slight abdominal distension after eating, tiredness, lassitude, dull-pale complexion, weakness of the limbs, loose stools, poor memory, thin body, scanty periods or amenorrhoea.
Tongue: Pale, Thin and slightly dry.
Pulse: Choppy or Fine.
Key symptoms: tiredness, slight abdominal distension, scanty periods, Pale tongue.
Acupuncture
Points: Ren-12 Zhongwan, ST-36 Zusanli, SP-6 Sanyinjiao, BL-20 Pishu, BL-21 Weishu, Ren-4 Guanyuan, BL-17 Geshu (with direct moxa).
Method: reinforcing method. Moxa is applicable.
THE ZHI OF THE KIDNEYS
The word Zhi has at least three meanings:
1. it indicates "memory"
2. it means "will power "
3. it is sometimes used to indicate the "five Zhi", i.e. the five mental aspects Shen, Hun, Po, Yi and Zhi itself.
In the first sense, the Kidneys influence our capacity for memorizing and storing data. Some of the ancient doctors even said that the Yi of the Spleen and the memory of the Kidneys are almost the same thing, except that the Yi is responsible for memorizing in the course of studying and the Zhi of the Kidneys is responsible for the storing of data over the long term.
Tang Zong Hai says: "Zhi indicates Yi with a capacity for storing [data]".
The character for Zhi is indicated below. It is composed of Shi on the upper part and the "Heart" in the lower part.

KIDNEY-YIN DEFICIENCY
Dizziness, tinnitus, vertigo, poor memory, hardness of hearing, night-sweating, dry mouth and throat at night, lower backache, ache in bones, dark-scanty urine, infertility, premature ejaculation, tiredness, lassitude, slight anxiety.
Tongue: normal-coloured without coating.
Pulse: Floating-Empty.
Key symptoms: backache, night sweating.
Acupuncture
Points: Ren-4 Guanyuan, KI-3 Taixi, KI-6 Zhaohai, KI-10 Yingu, KI-9 Zhubin, SP-6 Sanyinjiao, Ren-7 Yinjiao, LU-7 Lieque and KI-6 Zhaohai in combination (opening points of the Ren Mai).
Method: reinforcing method, no moxa.
In the sphere of thinking, remembering and memorizing there is considerable overlap between the Yi of Spleen, the Shen of Heart and the Zhi of Kidneys. The main differentiating factor is that the Spleen is responsible for memorizing data in the course of one's work or study.
For example, it is not uncommon for someone to have a brilliant memory in his or her field of study or research (a function of the Spleen), and yet be quite forgetful in daily life (a function of the Heart).
The Heart and Kidneys also contribute to this function, but they are also responsible for the memory of past events and implicit memory. In particular, the overlap between the Yi and the Shen in thinking activity is very close, so much so that the "Ling Shu" says in chapter 8: "The Heart function of recollecting is called Yi".
In turn, the memorizing function of the Yi is so closely related to the Zhi of the Kidneys that the same chapter continues: "The storing [of data] of the Yi is called Zhi".
These passages confirm that Shen, Yi and Zhi are a continuum.
Memory and sense of Self
In modern psychology, "memory" is more that just the ability to store facts and information in our brain. It is actually an essential part in which our consciousness exists, works and manifests itself and working memory plays an important role in our consciousness.
Even the thought "I live in the present" requires short-term memory. Even the immediate present requires involves memory - what we know about the one present moment is basically what is in our working memory.
Working memory allows us to know that the "here and now" is "here" and is happening "now". This insight underlies the notion, adopted by a number of cognitive scientists, that consciousness is the awareness of what is in working memory.
LeDoux says: "The self is in part made and maintained by memory and both implicit and explicit forms are involved."[1]
Thus, in a broader sense, Zhi is much more than "memory" in the sense of being able to remember past events. The Zhi (together with the Shen) contributes to our working memory and also to the long-term memory. Together with the Shen of the Heart, this contributes to creating our consciousness and sense of self.
Treatment of poor memory

Memory can be stimulated by treating:
Heart (Shen): HE-7, HE-3, BL-15, BL-44 Shentang
Kidneys (Zhi): KI-3, BL-23, BL-52 Zhishi
Spleen (Yi): SP-3, BL-20, BL-49 Yishe
Du Mai (Brain/Sea of Marrow): SI-3/BL-62, Du-16, Du-20.
The Du Mai and memory
Another factor in memory is the Du Mai for three reasons.
1) It flows through the Heart and therefore affects Shen.
2) It originates from the Kidneys and therefore affects Zhi.
3) It is the vessel through which the Kidneys' Sea of Marrow reaches the Brain.
The three main points are Du-11 Shendao, Du-20 Baihui and Du-24 Shenting.
The Lungs and memory
However, remember that there are other factors at work in memory, e.g. the Lungs affect memory by regulating the amount of Qi reaching the head.
Thus LU-7 and LU-3 are important for poor memory due to Qi not reaching the head.
The "Explanation of the Acupuncture Points" says that LU-3 can make Qi rise to treat forgetfulness, sadness and weeping due to Qi not rising to head.[2]
Forgetfulness is an important indication for this point: this is forgetfulness due to clear Qi not rising to the head. According to the "Explanation of the Acupuncture Points", this point treats forgetfulness by stimulating the ascending of Qi of both Lungs and Heart.[3]
Phlegm and Blood stasis in memory
Finally, it is important to remember that memory is affected by Full conditions, especially Phlegm and Blood stasis obstructing the Brain. This happens especially in the elderly.
In particular, Phlegm is a common cause of poor memory: when it is, poor memory is accompanied by dizziness and a feeling of heaviness and muzziness (fuzziness) of the head. The tongue is swollen.
Points for Phlegm obstructing the Brain and affecting memory are: Du-20 Baihui, Du-24 Shenting, ST-40 Fenglong, LU-7 Lieque, Ren-9 Shuifen, Ren-5 Shimen, BL-22 Sanjiaoshu, P-5 Jianshi.
END NOTES
[1] Joseph Ledoux, The Emotional Brain, Simon and Shuster, NY, 1996, p. 278.
[2] An Explanation of the Acupuncture Points (Jing Xue Jie), pp. 26-7.
[3] Ibid., p. 27.
By: Giovanni Maciocia
Hyperthyroidism and Hypothyroidism
Safe and effective treatments for Thyroid Disorders
There are two main thyroid disorders: hyperthyroidism and hypothyroidism. Hyperthyroidism is a condition in which the thyroid gland is overactive and produces too much thyroid hormone. Typical symptoms of hyperthyroidism include: high blood pressure; fast heartbeat; moist skin; increased sweating; tremor; nervousness; increased appetite with weight loss; diarrhea and/or frequent bowel movements; weakness; eyes that seem to bulge out of their sockets; and sensitivity of the eyes to light. Hypothyroidism is a condition in which the thyroid gland is under-active and produces too little thyroid hormone. Typical symptoms of hypothyroidism include: hoarse voice; slowed speech; puffy face; drooping eyelids; intolerance of cold conditions; constipation; weight gain; dry hair; dry skin; and depression.
Thyroid Disorders in Chinese Medicine
 In traditional Chinese medicine, both hyperthyroidism and hypothyroidism are considered to be a Yin/Yang imbalance. In Chinese philosophical and medical theory, Yin and Yang are the essential components of the material universe. Everything that exists is Yin or Yang (generally a combination of both in a characteristic balance). The Yin principle is dark, moist, receptive, female, sinking, and its electrical charge is negative. The Yang principle is light, fiery, active, male, outward-expanding, and its electrical charge is positive. A very basic principle of Chinese medicine is to keep the Yin and Yang in balance, since the balance of Yin and Yang represents the healthy state of the body. A treatment intervention by traditional Chinese medicine (which includes acupuncture, herbal medicine, and dietary therapy) is designed to bring the Yin and Yang back to a normal balance. In Western terms, an overproduction or underproduction of thyroid hormone alters the body s chemical balance and causes hyper- or hypothyroidism. In Chinese terms, when Yin is deficient it cannot control the Yang energy from escaping outward and upward, and this "reckless" movement of Yang brings about the characteristic symptoms of hyperthyroidism. When Yang is deficient, it simply cannot produce the vital energy necessary to keep the body functioning well, and symptoms of hypothyroidism result.
In traditional Chinese medicine, both hyperthyroidism and hypothyroidism are considered to be a Yin/Yang imbalance. In Chinese philosophical and medical theory, Yin and Yang are the essential components of the material universe. Everything that exists is Yin or Yang (generally a combination of both in a characteristic balance). The Yin principle is dark, moist, receptive, female, sinking, and its electrical charge is negative. The Yang principle is light, fiery, active, male, outward-expanding, and its electrical charge is positive. A very basic principle of Chinese medicine is to keep the Yin and Yang in balance, since the balance of Yin and Yang represents the healthy state of the body. A treatment intervention by traditional Chinese medicine (which includes acupuncture, herbal medicine, and dietary therapy) is designed to bring the Yin and Yang back to a normal balance. In Western terms, an overproduction or underproduction of thyroid hormone alters the body s chemical balance and causes hyper- or hypothyroidism. In Chinese terms, when Yin is deficient it cannot control the Yang energy from escaping outward and upward, and this "reckless" movement of Yang brings about the characteristic symptoms of hyperthyroidism. When Yang is deficient, it simply cannot produce the vital energy necessary to keep the body functioning well, and symptoms of hypothyroidism result.
Recent research, by both Western and Chinese scientists, offers several exciting theories to reinforce ancient ideas about Yin and Yang balance in the body.
Patterns and Treatment of Thyroid Disorders in Chinese Medicine
Hyperthyroidism Three patterns of Yin Deficiency are differentiated for hyperthyroidism: Kidney Yin Deficiency with Excess Heat; Heart/Liver Yin Deficiency; and Heart/Kidney Yin Deficiency. In the pattern of Kidney Yin Deficiency with Excess Heat, typical symptoms are: enlarged, soft, smooth thyroid; anxiety; anger; aversion to heat; flushed, warm face; dry mouth with a bitter taste; increased appetite; bulging eyes; tremor; increased volume of bowel movements, a red tongue body with a dry, yellow coating; and a wiry, rapid pulse.
In the pattern of Yin Deficiency with Heart and Liver Deficiency, the symptoms are: enlarged, swollen, soft, smooth thyroid; heart palpitations; anxiety; insomnia; increased appetite with weight loss; dry throat; a red tongue body with a yellow tongue coating or no coating; and a thin, rapid pulse.
In the pattern of Yin Deficiency with Heart and Kidney Deficiency, common symptoms are: enlarged, swollen thyroid; hand tremors; dry mouth and eyes; heart palpitations; increased appetite; irregular period or amenorrhea (for women); impotence or low sex drive (for men); weakness of the knees and lower back; a red tongue body without coating, and a deep, thin, rapid pulse.
Kidney Yin Tonic (Liu Wei Di Huang Wan) is the herbal formula most commonly used for the symptoms of hyperthyroidism. Other herbal formulas, such as Heart Yin Tonic (Tian Wang Xin Bu Dan) are also used, depending on the specific pattern.
Hypothyroidism Two patterns of Yang Deficiency are differentiated for hypothyroidism:: Spleen/Kidney Deficiency, and Heart/Kidney Deficiency. In the pattern of Yang Deficiency with Spleen and Kidney Deficiency, the key symptoms are: lassitude; sleepiness; poor memory; dizziness; ringing in the ears (tinnitus); weakness of the lower back and knees; aversion to cold; dry skin; dry hair; constipation; edema; impotence (men); irregular periods (women); pale, puffy tongue body with tooth marks along the edge; white, sticky tongue coating; and a pulse that is deep and thin or deep and slow.
In the pattern of Yang Deficiency with Heart and Kidney Deficiency, the characteristic symptoms are: heart palpitations; chest congestion and pain; sleepiness; feeling cold; pale, tender tongue body with a white, slippery coating; and a deep, slow pulse.
Kidney Yang Tonic (Jin Gui Shen Qi Wan) is the leading herbal formula for treating the symptoms of hypothyroidism. Formulas such as Right Restoration Formula You Gui Wan are also widely used.
FOCUS ON A REMEDY: WARM THE MENSES
Warm the Menses is a variation of the well-known classical prescription Wen Jing Tang Warming the Menses Decoction by Zhang Zhong Jing (AD 150-219) from his book Jin Gui Yao Lue (Essential Prescriptions of the Golden Cabinet).
The original prescription is as follows:
Wu Zhu Yu Fructus Evodiae rutaecarpae
Gui Zhi Ramulus Cinnamomi cassiae
Dang Gui Radix Angelicae sinensis
Chuan Xiong Rhizoma Chuanxiong
Bai Shao Radix Paeoniae alba
E Jiao Gelatinum Corii Asini
Mai Men Dong Tuber Ophiopogonis
Mu Dan Pi Cortex Moutan radicis
Ren Shen Radix Ginseng
Ban Xia Rhizoma Pinelliae preparatum
Gan Cao Radix Glycyrrhizae uralensis
Sheng Jiang Rhizoma Zingiberis officinalis recens
The rationale behind it is as follows. When Cold obstructs the Uterus, it makes Blood stagnate. When Blood stagnates, new Blood has nowhere to go and it cannot be contained in the Uterus: this induces a deficiency of Blood.
A long-standing Blood deficiency may give rise to some Empty Heat signs, which may mistakenly be interpreted as Heat signs; but the Pale-Purple colour of the tongue clearly indicates that this is not so. In fact, the original text refers to a parched mouth and lips as the symptoms of Empty Heat from Blood deficiency.
When used for its proper pattern of long-standing internal Cold occurring against a background of Deficiency and leading to stasis of Blood, this formula is very effective. An essential sign for its use is that the tongue-body colour be Pale or Bluish-Purple.
Explanation
- Wu Zhu Yu, Gui Zhi and Sheng Jiang warm the Uterus and expel Cold.
- Dang Gui, Chuan Xiong and Bai Shao nourish and invigorate Blood, which is necessary because the obstruction of the Uterus by Cold prevents new Blood from taking its proper place there.
- Ren Shen tonifies Qi to nourish Blood.
- Mai Men Dong and E Jiao nourish Blood and Yin.
- Mu Dan Pi clears any Empty Heat which might arise from Blood deficiency.
- Ban Xia harmonizes the Uterus via the Stomach channel to which it is connected through the Chong Mai.
- Gan Cao harmonizes. The following are the ingredients of Warm the Menses:
The following are the ingredients of Warm the Menses:
Wu Zhu Yu Fructus Evodiae
Gui Zhi Ramulus Cinnamomi cassiae
Rou Gui Cortex Cinnamomi
Dang Gui Radix Angelicae sinensis
Chuan Xiong Rhizoma Chuanxiong
Bai Shao Radix Paeoniae alba
Dang Shen Radix Codonopsis
Mai Men Dong Radix Ophiopogonis
Mu Dan Pi Cortex Moutan radicis
Ban Xia Rhizoma Pinelliae preparatum
Zhi Gan Cao Radix Glycyrrhizae uralensis preparata
Shu Di Huang Radix Rehmanniae preparata
Yan Hu Suo Rhizoma Corydalis
Wu Yao Radix Linderae
Yi Mu Cao Herba Leonuri
Du Zhong Cortex Eucommiae ulmoidis
Patterns: Stagnation of Cold in the Uterus, stasis of Blood, Blood deficiency, Kidney-Yang deficiency.
Actions: Expel Cold, warm the Uterus, invigorate Blood, eliminate stasis, nourish Blood, tonify and warm Kidney-Yang.
Indications: very painful periods with pain of a spastic character that is alleviated by the application of heat (such as a hot-water bottle), red or dark menstrual blood with small, dark clots, a pronounced feeling of cold that is aggravated during the period, late periods, irregular periods, infertility from Cold obstructing the uterus, bright-pale complexion, weariness, tiredness, backache, frequent pale urination, occasionally a slight feeling of heat in the face and a dry mouth or lips.
Tongue: Pale, wet.
Pulse: Deep, Tight, slow.
IN A NUTSHELL: expel Cold from the Uterus, invigorate Blood, nourish Blood, tonify Kidney-Yang. The two main indications for this remedy are painful periods and infertility from Cold in the uterus.
The main differences from its classical antecedent are that it tonifies Kidney-Yang and it invigorates Blood.
By Giovanni Maciocia
Treating Insomnia With Chinese Herbal Medicine
Treating Insomnia With Chinese Herbal Medicine
Insomnia, or the inability to fall asleep or remain asleep, has been and continues to be treated using  CHM to the present day.
CHM to the present day.
A recent study in Evidence-based Complementary and Alternative Medicine evaluated and reviewed the use of CHM for insomnia treatment in Taiwan. The study showed that there were 16,134 subjects who visited traditional Chinese Medicine clinics for insomnia in Taiwan during the year 2002. In addition, several studies have demonstrated that CHM treatments effectively benefit sleep quality, improve sleep duration, and exhibit reduced side effects in comparison to Western medicines.
One of the most efficient formulas is the "Resolve & Stabilize", indicated for the treatment of recalcitrant insomnia which has lasted for more than three months. It can be used when other, more conventional Chinese therapies for insomnia have failed. Patients may not be able to sleep at all or only 1-2 hours per night.
Research outcomes:
In 38 patients with recalcitrant insomnia lasting for more than three months, 23 were cured, 12 improved, and only three got no effect, for a total amelioration rate of 92.1%. The shortest course of treatment was 10 days, the longest was 49 days.
The most commonly prescribed Chinese herbal formula for insomnia was Suan Zao Ren Tang. This formula consists of 5 individual herbs grouped together for the most beneficial synergistic effect. The primary herb in this formula is Ziziphus spinosa, or Suan-zao-ren (a.k.a., sour jujube seed). This herb has been shown to cause a sedative effect at higher doses and an anxiolytic effect at lower doses.
Another study found that the formula Suan Zao Ren Tang produced an increase in non-rapid eye movement sleep, and it is believed that the mechanism was by the stimulation of serotonin receptors. The other herbs in this formula include Chuan-xiong (Szechuan lovage root), Fu-ling (poria), Zhi-mu (anemarrhena rhizome), and .jpg) Gan-cao (licorice root).
Gan-cao (licorice root).
It is important to note that whereas Western medicine attempts to treat insomnia as an isolated symptom, traditional Chinese medicine examines the condition of the body as a whole system, taking into consideration signs and symptoms ranging from appetite, thirst, mood, tongue color, and the quality of the pulse to reach a diagnosis.
Suan Zao Ren adults
Suan Zao Ren pediatrics
Cordyceps Sinensis research
Cordyceps sinensis, or commonly known as catepillar fungus and dong chong xia cao (冬蟲夏草) in Chinese, is an expensive traditional Chinese medicine well-known for its anti-tumour, immunostimulant and antioxidantfunctions. The catepillar fungus has also been proven to be anti-diabetic.
The catepillar fungus has been used hundreds of years in TCM to boost the immune system of those who eat it. This is why after the outbreak of SARS in Hong Kong in 2002, the price of the fungus shot up to US$7,000/kg, half the price of gold. And the over heavesting of the fungus has significantly threatened the ecology of the Bhutanese wilderness.
What is Cordyceps sinensis? Cordyceps sinensis has long been used in folkmedicine throughout Asia. It has been used as an important nourishing tonic.
A kind of mold, cordyceps sinensis spawn invades into the body of a silkwormwhich is an insect and grows, multiplies making the protein of the insect its source of nutrition and makes the host insect a mummy. Passing by winter,Cordyceps sinesis forms a fruit body in the epidermis of the insect at the time when a temperature and a humidity becomes high and it becomes a mushroom. It has only been in the last few years however that science has had the ability to thoroughly analyze this mushroom, and identify the bioactive compounds present.
To prove the value of the catapillar fungus, one study found that a polysaccharide isolated from cordyceps sinensis protects PC12 cells, a cell line derived from an adrenal glandtumour, against hydrogen peroxide-induced injury.
The study was done by scientists from the Institute of Chinese Medical Sciences at the University of Macau Department and from the First Affiliated Hospital of Anhui Medical University.
The isolated polysaccharide, named CSP-1, which has strong anti-oxidation activity, contains glucose, mannose and galactose in the ratio of 1:0.6:0.75.
The researchers found that CSP-1 can significantly reduce blood glucose levels in diabetic mice. CSP-1 may stimulate pancreatic release of insulin and/or reduce insulin metabolism.
Another study done at the Department of Chemical Pathology of the Chinese University of Hong Kong established the biological functions of the fungus. The researchers used a cultivated strain of the caterpillar fungus to describes its immunomodulatory features through a series of in vitro and in vivo experiments. The researchers claim that this was the Bhutanese wilderness.
In vitro results demonstrated that the fungus induced the production of various cytokines and the tumour necrosis factor alpha (TNF-α). It also mobilized the alien fighters lymphocytes and monocytes. These are all key players in our immune system.
What are macrophages? Macrophages are cells within the tissues that originate from specific white blood cells called monocytes. Monocytes and macrophages are phagocytes, acting in both nonspecific defense (or innateimmunity) as well as specific defense (or cell-mediated immunity) of vertebrate animals. Their role is to phagocytize (engulf and then digest) cellular debris and pathogens either as stationary or mobile cells, and to stimulate lymphocytes and other immune cells to respond to the pathogen.
What are cytokines? Cytokines are a group of proteins and peptides that are used in organisms as signaling compounds. These chemical signals are similar to hormones and neurotransmitters and are used to allow one cell to communicate with another. While hormones are released from specific organs into the blood and neurotransmitters are released by nerves, cytokines are released by many types of cells. They are particularly important in both innate and adaptive immune responses. Due to their central role in the immune system, cytokines are involved in a variety of immunological, inflammatory and infectious diseases.
What is tumour necrosis factor? Tumour necrosis factor is a protein produced by several of the body’s cell types, such as white blood cells, red blood cells, and other cells that line the blood vessels. It promotes the destruction of some types of cancer cells. In addition to tumour cell-killing activity, TNF-α has been noted for its role in the inflammatory response and the body’s resistance to pathogens. Moreover, the use of pure recombinant TNF-α has demonstrated that this cytokine can inhibit the replication of several viruses including the influenza virus.
Cordyceps Sinensis practical uses:
- It stimulates sexual desire (in women and men)
- Chronic fatigue or tiredness, feelings of extreme weakness. It is also used to improve athletic performance.
- Tonifies the sexual energy and has been used for impotence, espermatorrea, frigidity, etc..
- Strengthens the immune system. It helps our body fight different bacteria. Makes a natural antibiotic function.
- It was given anti-inflammatory properties and therefore very often mentioned, in traditional Chinese medicine for its use in cases of rheumatism, arthritis, lumbago.
- Strengthens the respiratory system and makes the role of mucolytic and antitussive. Used to treat asthma, bronchitis, respiratory failure, emphysema, tuberculosis.
- Can be supportive in the fight against cancer because it increases the resistance of the patient at the same time it strengthens the immune system.
- Allied of the circulatory system. It favors a good peripheral and cerebral blood flow, it is recommended in case of lack of memory, dizziness, cold feet, etc.
Chinese Herbal Medicine for Panic Attacks
If you have never had a panic attack, you cannot imagine the minutes or possibly hours of sheer terror that the person having one can experience. The typical medications used are anti-anxiety medications that do help ease or prevent anxiety, but can dull the person's mental state and can lead to physical dependence. In complete contrast to this, Chinese herbal medicine can help reduce the chances of a person having a panic attack, without the risk of unnecessary and unpleasant side effects. Chinese herbal medicine can build a comfort level in the body and nourish one's emotional and mental state, to prevent panic attacks from happening.
It is believed by many experts that mental and nervous exhaustion can make certain people prone to panic attacks and high levels of anxiety. Chinese herbal medicine can help nourish this mental and nervous fatigue, creating a feeling of well-being and calmness. In addition, there are many herbs that can promote an immediate feeling of calm and peace, to help bring one down from a panic attack.
If you have been diagnosed with an anxiety/panic disorder, your doctor is more than likely going to prescribe a mild sedative for you and recommend that you seek the services of a licensed therapist, to help you learn how to regain control of your life. While the therapist is a good idea as he can teach you relaxation techniques such as meditation and deep breathing exercises, the medication may not be a permanent option. Benzodiazepines are commonly prescribed such as Xanax (alprazolam), Klonopin (clonazepam), Valium (diazepam), Ativan (lorazepam). These drugs can help a person in that horrible anxious state, but they are merely a band-aid. Of course, lifestyle changes, learning new ways to deal with stress, being on a proper exercise program, eating healthy and nourishing foods, proper sleep, and taking the right supplements such as Chinese herbal medicine, can help a person truly heal from anxiety disorder or frequent panic attacks.
Benzodiazepines can cause drowsiness, light headedness, memory loss, nausea, and some people, especially on long term use can feel depressed. On the contrary, the proper Chinese herbal medicine formula to treat anxiety and panic attacks should have no side effects.
Natural Happiness
Chinese herbal medicine has been used for thousands of years to cure any number of ailments, so it should come as no surprise, that there is an herbal remedy available that can help to reduce panic attacks in someone diagnosed with an anxiety/panic disorder.
For almost one thousand years the herbal remedy called Rambling Powder (XIAO YAO SAN) , has been used to calm one's nerves and release tension. The goal of this formula was to foster a feeling of a free rambling spirit, with no tension, proceeding through life with ease. First recorded in 1638, another Chinese remedy, The Heavenly Emperor's Heart Nourishing Pills TIAN WANG BU XIN Dan has been used for centuries to calm restlessness and agitation, while nourishing the spirit. The ancient Chinese called this, "Calming and nourishing one's spiritual heart." Isn't that just how anxiety or a panic attacks feels? One's spiritual heart is in full agitation and the rug has been lifted up from under them. When your emotions and spiritual heart feels grounded, calm and nourished, anxiety is kept out. Combining these two formulas has been found to be very effective in helping those who suffer from panic attacks.
The most important thing to remember with all Chinese herbal medicine is that they are based on the knowledge accumulated over thousands of years and are made from 100% all natural pure ingredients. In most cases there are no known side effects and the scientific community is finally beginning to recognize their effectiveness.
Article Source:
Jeremy Speiser, L.Ac.
Master Herbalist
Clinical application of the Clear Metal remedy for advanced stage of influenza
Wind-Heat invasions can be of two types: it may be what I call a "simple" Wind-Heat invasion, or it may be a Wind-Heat invasion of the Wen Bing type. For example: an acute mononucleosis would be a Wind-Heat invasion of the Wen Bing type.
From the pathology point of view, they are basically the same, but the Wen Bing Wind-Heat invasions are more severe and potentially more harmful.
The " Clear Metal " remedy can be used for both types of invasions. Whether the Wind-Heat invasion is Wen Bing or not, I always make a diagnosis based on the theory of the "4 levels": Wei, Qi, Ying and Xue. I think that the theory of the 4 levels is absolutely essential for the diagnosis and treatment of acute wind-heat invasions.
At the Wei level, the Wind-Heat is on the outside. The Wei level is characterized by a simultaneous aversion to cold and fever. That is to say, you observe the patient, maybe he is a child in bed, he has a fever and his forehead is very hot, but the child feels cold. This is the classic symptomatology of the acute state of a Wind-Heat invasion, which would be at the Wei level, of the 4 levels. "Clear" Metal "is NOT for the Wei level, I repeat: It's not for the Wei level.
At the Qi level, Heat has penetrated the interior, and the main difference is that the patient no longer has an aversion to cold. He no longer feels cold, but warmth. The child is in bed, you are going to check the child, and you notice that the child is sweating, and has removed the covers. This means that the Heat has penetrated to the next level, that is, to the Qi level, in which the patient still has a fever, but feels hot and thirsty, possibly sweating, and, generally, at this level Qi, the Heat It is in the lungs. So there is, either Heat in Lung, or Phlegm-Heat in Lung, and, then, there would be cough, with or without expectoration. The " Clear Metal " remedy is for this level, for Heat at the Qi level, which would be the second stage of a Wind-Heat invasion.
Another characteristic of Wind-Heat invasions, especially those of the Wen Bing type, is that they progress rapidly. So we have to see the patient more than once a day, because we must change the treatment as soon as the pathogenic factor goes from the Wei level to the Qi level, which is characterized, I repeat, by the fact that the patient is no longer feels cold, but feels hot. When this happens, we can use "Clear Metal", especially if the Heat is pronounced.
" Clear Metal " should be administered in a relatively high dose of, at least, 9 tablets a day. If the patient has clear symptoms of Phlegm-Heat in Lung, that is Heat in Lung with Phlegm, then the remedy to be used, more than "Clear Metal", would be "Ringing Metal" [Resonating Metal]. These two remedies are similar in that they treat the Qi level, but "Clear Metal" is better if the Heat is pronounced: the patient is very hot, thirsty and dry in the mouth. If the patient has cough with expectoration of mucus, then we can use the "Ringing Metal" remedy.
In summary, these two remedies are similar, in the sense that both treat the Qi level, but "Clear Metal" is especially better if the Heat is pronounced, and "Ringing Metal" is better if there is Phlegm-Heat in the Lungs.
By the way, another reason to use " Clear Metal " is that, if the Heat is pronounced, it could also progress to the next level, that is, to the Ying level, which would be a bad progression, because, potentially, there could be serious repercussions in the Ying level or in the Xue level. So it is very important to treat the Heat at the Qi level, and stop it at the Qi level, with the use of " Clear Metal ".
by: Giovanni Maciocia
New Pediatric Formulas by "Blue Poppy"
We are proud to present the "Blue Poppy" Pediatric Formulas created by Bob Flaws;
Blue Poppy Pediatric Herbal tinctures offer condition-specific formulas in a glycerin base. With these formulas children take their herbs without complaint and they get better faster.
The Blue Poppy Pediatrics range of supplements provides you with a comprehensive range of products designed specifically with the infant in mind. From Allerase Jr. to Tummy Qi, Blue Poppy Originals offer a top quality blend of Western scientific research and Eastern traditions.
The squeeze dropper top of the herbal formula bottle is plastic in the case your child bites it! Safety first!
We all want the very best for our children and trying to keep them healthy and to support their short and long-term health can be challenging for any parent. Chinese traditional medicine has a rich history of over 2000 years of application. Using Chinese traditional herbal extracts and botanicals to support your children's health may be an appealing option, but trying to determine which herbs are best for your children can be daunting.
Blue Poppy Pediatrics range:
 AllerEase Junior
AllerEase Junior
Bupleurum & Angelica Formula
CQ Junior Fluid
Dry Nites Fluid
Little Pearl
Moisten Dryness
Peaceful Focus
Quiet Nites
Tender Teeth
Tummy Qi
BI SYNDROME
 This article looks in detail at "Bi" syndrome and the Three Treasures remedies which treat it. "Bi", also called "Painful Obstruction Syndrome" indicates pain, soreness, or numbness of muscles, tendons and joints. It is probably the most universal of all diseases affecting practically everyone at some time or another of one's life in all parts of the globe.
This article looks in detail at "Bi" syndrome and the Three Treasures remedies which treat it. "Bi", also called "Painful Obstruction Syndrome" indicates pain, soreness, or numbness of muscles, tendons and joints. It is probably the most universal of all diseases affecting practically everyone at some time or another of one's life in all parts of the globe.
"Bi", literally meaning "obstruction", can be caused by one or a combination of the following:
• invasion of external Wind
• invasion of external Cold
• invasion of external Dampness
However, in prolonged cases of Painful Obstruction Syndrome other pathological conditions may play a part in the development of the disease. First of all, Wind, Cold and Damp will obstruct the circulation of Qi, Blood and Body Fluids. After some time, Phlegm may develop. Phlegm may lead to stasis of Blood. The stasis of Blood in the channels further obstructs proper circulation and therefore is another cause of pain. In many cases of chronic Bi syndrome, stasis of Blood is a factor. For example, Cold and Dampness are frequent causes of Painful Obstruction syndrome of the lower back. After repeated episodes of invasion of the lower back by Cold and Dampness, the prolonged retention of pathogenic factors may lead to chronic stasis of Blood in the area. The ache then becomes more or less constant and more severe. Stasis of Blood also causes pronounced stiffness due to stagnant Blood not nourishing and moistening sinews.
Therefore, external Wind, Cold and Dampness may lead to:
• Qi stagnation
• Blood stagnation
• Phlegm
The above syndromes can (but do not always) occur against a background of Deficiency of either Qi, Yin, Yang or Blood.
DIFFERENTIATION OF BI SYNDROME
Wind Painful Obstruction Syndrome (Wandering Bi): caused by Wind and characterized by soreness and pain of muscles and joints, limitation of movement, pain moving from joint to joint.
Damp Painful Obstruction Syndrome (Fixed Painful Bi): caused by Dampness and characterized by pain, soreness and swelling in muscles and joints with a feeling of heaviness and numbness of the limbs, the pain being fixed in one place and aggravated by damp weather.
Cold Painful Obstruction Syndrome (Aching Painful Bi): caused by Cold and characterized by severe pain in a joint or muscle, limitation of movement, usually unilateral.
Heat Painful Obstruction Syndrome (Febrile Bi): originates from any of the previous 3 types when the pathogenic factor turns into Heat in the Interior. There is usually an underlying Yin deficiency. Characterized by pain and heat in the joints which feels hot to touch, redness and swelling of the joints, limitation of movement and severe pain.
Phlegm Painful Obstruction Syndrome (Bony Bi): Develops from any of the previous four types and is only ever chronic. Characterized by muscular atrophy, swelling and deformity of the bones in the joints. THE THREE TREASURES REMEDIES
THE THREE TREASURES REMEDIES
As always, a remedy must be prescribed only after a thorough case history has been taken, on the basis of the symptoms, pulse and tongue.
Clear Channels
Pattern: Damp-Heat in the joints, Blood stasis
Action: Drain Dampness, expel Wind, clear Heat, benefit the joints, invigorate Blood
Indications: sub-acute Painful Obstruction Syndrome from Damp-Heat, painful, swollen, hot and red joints, rheumatoid arthritis, gout
Tongue: Swollen with sticky-yellow coating
Pulse: Slippery, Rapid
Benefit the Sinews
Pattern: Blood stasis, Phlegm and Dampness in the joints, Kidney deficiency
Action: invigorate Blood, resolve Phlegm, expel Wind-Dampness, dry Dampness
Indications: chronic Bi, chronic joint pain with swelling of the joints and bone deformities, rigidity of joints
Tongue: Pale, red or purple, swollen, sticky coating
Pulse: Choppy or slightly Slippery
Brocade Sinews
Pattern: Chronic Wind-Damp Painful Obstruction (Bi) Syndrome with Liver-Blood and/or Liver-Yin deficiency
Action: Nourish Liver-Blood and Liver-Yin, benefit sinews, expel Wind-Dampness from the joints
Indications: Chronic soreness and slight swelling of the joints, dizziness, numbness or tingling or limbs.
Tongue: Pale and thin if there is Liver-Blood deficiency or red and thin without coating if there is Liver-Yin deficiency
Pulse: Choppy or Fine, possibly only on the left side.
Nourish the Root and Clear Wind
Pattern: chronic Wind-Damp Painful Obstruction (Bi) Syndrome occurring against a background of Kidney-Yin deficiency
Action: Nourish the kidneys and Liver, strengthen bones and sinews, expel Wind-Dampness in the joints
Indications: lower backache, knee-ache, sciatica, ache in joins
Tongue: Red without coating or with a rootless coating
Pulse: Weak on both rear positions or Floating-Empty

CASE HISTORIES
Case History 1
A 52-year old woman had been suffering from rheumatoid arthritis since the birth of her last child 17 years ago. Two months before she came for treatment, she had had a bad flare up. Her wrists, hands, knees, ankles and feet were extremely swollen and hot. She had a severe restriction of movement. Her pulse was Slippery-Rapid and her tongue was Red.
I diagnosed severe Damp-Heat in the joints with an underlying deficiency of Liver-Blood and Yin. I prescribed 9 tablets of Clear Channels a day to treat the Manifestation, and gave her acupuncture to treat the underlying deficiency. After 3 months, the flare-up had subsided. The joints were less swollen and hot and the patient’s mobility was less restricted.
Case History 2
A 64-year old woman had been experiencing a lot of pain in the fingers of both hands for the past year. On top of this, the fingers were swollen and quite deformed. She also complained of frequent lower backache and a weak feeling in her knees. She said she felt very stiff on waking in the morning and this feeling eased off gradually as the day went on but never quite left her. Her tongue was Pale and partially Peeled and her pulse was slightly Floating-Empty.
The pain and deformity in her fingers and handsrobably began as an invasion of Cold and Dampness but, over the year, turned into stagnation of Phlegm. There is an underlying deficiency of Blood (seen in the Pale tongue) and Yin (the tongue is partially peeled and the pulse Floating-Empty). The back and knee problems also point towards Kidney-Yin deficiency. I prescribed 6 Benefit the Sinews a day and after six months the condition was ninety percent better.
Case History 3
A 57-year-old woman had been suffering from chronic lower backache for the past ten years. An MRI scan had shown a severe deterioration of the intervertebral discs. Her backache was worse with exercise and better with rest. She also complained of hot flushes and nightsweats. Her tongue was slightly Red and completely without coating with some cracks in the central area. Her pulse was Slippery, and Weak on both Rear positions.
I diagnosed Kidney- and Liver-Yin deficiency and prescribed 6 tablets of Nourish the Root and Clear Wind a day. Given the severe deterioration of the intervertebral discs, this backache could not be cured completely but the continuous administration of the above remedy greatly relieved the pain and allowed her to lead a normal life.
By Giovanni Maciocia


